Endometriosis is a condition where tissue that is somewhat similar to the lining of the uterus (the endometrium) is found outside the uterus where it does not belong. Endometrial secretions irritate the surrounding tissues. The immune system responds causing swelling, inflammation and severe pelvic pain.
Endometriosis is one of the most common gynecological diseases, according to the National Institute of Child Health and Human Development (NICHD). It is estimated that around 1 in 10 women are affected by endometriosis, which equates to some 176 million women worldwide. Endometriosis does not discriminate against age, ethnicity or socioeconomic status. It can affect women from every walk of life and in every life-phase: teenage schoolgirls, mothers, women who have put off having children, and women post-menopause. The disease can impact upon all aspects of a girl or woman’s quality of life. Many women suffer for years and visit multiple doctors before finally receiving a diagnosis. The diagnostic delay from the onset of symptoms to diagnosis ranges in average from 7 to 10 years. Endometriosis is a medical condition where the endometrium tissue is found outside the uterus where it does not belong. This abnormal tissue contains endometrial glands and stroma. The glands secrete substances that irritate the surrounding tissues, sometimes causing them to bleed. The immune system responds to the release of these substances by releasing inflammatory proteins that rush to the site of disease, causing swelling and inflammation. The disease itself and the inflammatory response to the disease can cause the patient severe pelvic pain. Over time, scar tissue may form and bands of scarring may develop, sticking the pelvic organs together (adhesions).
Endometriosis does not discriminate against age, ethnicity or socioeconomic status. It can affect women from every walk of life and in every life-phase.

It is estimated that around 1 in 10 women are affected by endometriosis, which equates to some 176 million women worldwide.
What are the symptoms of Endometriosis?
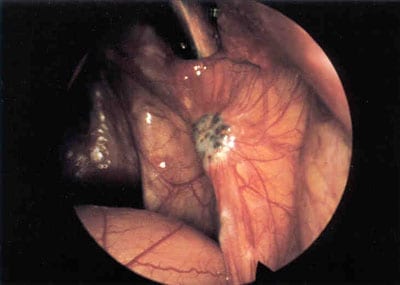
Endometriosis may be suspected if a woman is suffering from pelvic pain, cyclical pain, painful sex, painful bowel movements, painful urination and/or gastrointestinal symptoms. GI symptoms can include diarrhea, constipation, nausea, gassiness, bloating and intestinal cramping pain. During the pelvic exam, the patient may report specific areas of tenderness and pain. The physician may detect nodularity behind the patient’s uterus. An actual diagnosis is only possible via surgery, where biopsies are obtained of any areas of abnormal tissue, sent to a pathologist for microscopic inspection and the presence of endometrial-like glands and stroma are confirmed.
Further Reading: “What are the common endometriosis symptoms?”
How to Properly Treat Endometriosis

Optimal care starts by sitting down and really listening to the patient. Too many doctors fail to listen to what their patients have to say about their own bodies.
-Dr. Cook
If you have endometriosis, finding the right treatment can be confusing and you may be asking many questions such as, “How can my endometriosis best be treated?”, “What are my treatment options?”, “What kind of doctor can provide me with the best endometriosis treatment?” You may have heard conflicting or outright inaccurate information about the treatment options available, everything from simply just taking birth control pills to treat your endometriosis symptoms, all the way to being told you have to get pregnant or have a hysterectomy to treat or cure your endometriosis. Obviously, the most appropriate treatment will depend on the severity of your endometriosis and the nature of your symptoms (pain and/or infertility) and the presence of other associated health conditions. Relieving you of your symptoms of endometriosis and restoring your health requires both an extensive knowledge of the condition as well as the experience and expertise needed to offer you the best treatment.
To treat endometriosis we need to know what we are dealing with
The true nature of endometriosis has eluded the medical community for centuries. The cause of the disease remains uncertain; said simply, many different factors (genetic, developmental and environmental) have been implicated in the course and nature of this condition.
So what do we know?
- No two endometriosis patients are alike. Endometriosis varies widely in appearance, location and severity. The effects of the disease on the body differ between individuals and within the same individual throughout life.
- The effects of endometriosis can be both local (pelvic pain) and systemic (affecting multiple organs and systems throughout the body).
- Endometriosis is frequently accompanied by other gynecological, immunological, and endocrine disorders. As a result, meticulously removing the disease, while an essential step in the journey to recovery, is just one component in a proactive integrative approach to improving your overall health.
Our unique approach utilizes specialized surgery in combination with non-surgical traditional western and integrative treatments to address all aspects of endometriosis and its associated conditions on the body.
Why have my previous treatments failed to help?
Previous treatments may have failed or only partially helped for several reasons:
Surgery was unsuccessful in completely eradicating the disease. This may be due to areas of disease being overlooked, failure to treat areas of disease that overlie delicate or vital structures, and using techniques that only partially destroy the disease. If any endometriosis remains after surgery, the patient’s pelvic pain may persist or recur. Endometriosis surgery is complex and specialized, and requires the expert skill and experience of a surgical specialist.
In many cases, doctors rely on hormone therapy rather than surgery, inducing a state of pseudo-pregnancy or pseudo-menopause in the patient. Hormone therapies are often poorly tolerated due to the significant side effects they produce and may only be partially effective in managing a patient’s pain. They do not make the disease go away, they at best offer palliative care, and they are not suitable for patients struggling with infertility.
Even if a patient has previously undergone the successful surgical removal of her disease and has no remaining endometriosis, she may experience persistent pain and other systemic symptoms. In many patients, the symptoms attributed to endometriosis are in fact multifactorial in origin. Continuing symptoms can result from the secondary effects of endometriosis and its treatment, such as ongoing side effects of previous hormone therapies (e.g. Lupron) or from post-operative adhesions. Another explanation for ongoing pain is the presence of separate (yet sometimes related) health conditions, such as adenomyosis, pudendal neuralgia, interstitial cystitis, pelvic floor dysfunction, vulvar vestibulitis, irritable bowel, allergies and intolerance or sensitivity to certain foods, thyroid dysfunction, fibromyalgia, chronic fatigue, centralized sensitization and neuropathic pain, and the psychological toll of chronic pain. Excellent surgery can remove the disease and bring about relief but may not address the “evil siblings” of endometriosis.
While these are some of the common culprits of treatment failure, there is no cookie cutter answer to this question, which is why a thorough medical history, record review and patient narrative are needed to uncover the possible factors in your continued symptoms.
Combining knowledge with expertise to offer the best treatment
Drawing upon a deep understanding of endometriosis, treatment at Vital Health involves the following key steps:
First, we listen to you and take an acute interest in every aspect of your current health and medical history. This is the only way to truly know why previous treatments have failed and how we can do things differently. During this process, we consider the entire body: pelvic disease and adhesions, fertility, diet and nutrition, allergies, stress, cognition and pain psychology, exercise, co-existing medical conditions, familial risk factors, and exposure to environmental toxins
The medical history analysis is followed by a thorough physical, pelvic and ultrasound exam to map out any areas of pain, tenderness and/or nodularity, and identify any signs of pelvic and systemic disease.
Based on these findings, we consider possible plans of action. As a patient, your preferences and decisions are integral to your personal treatment plan. We work as a multidisciplinary team to decide which treatments are best for you, with your thoughts and wishes central.
Meticulous surgery to diagnose and carefully remove all endometriosis present can be combined with specialized in-office treatments and therapies tailored to the unique needs of endometriosis patients: pelvic physiotherapy, nutrigenomics and nutritional counseling, pain psychology and psychotherapy, pain management, and gynecologic management and treatment of associated conditions of the uterus, vulva, bowel, bladder, pelvic floor, and pelvic nerves.
For our patients from further afield, we offer many of these specialized services in the form of long-distance consultation and follow-up.
Our care and concern for your health is ongoing. During the first days, weeks and months after surgery, each patient is carefully followed up via in-office and phone consults. Thereafter we invite you to provide yearly feedback on how you are doing and our door always remains open should you require additional treatment or simply a listening ear.
We firmly believe that there is hope for each and every woman with this debilitating disease. Patients have come to us for successful treatment after having had up to 20 previous failed surgeries. There is no such thing as an inoperable or untreatable case of endometriosis; we will not turn you away and we are truly dedicated to doing all we can to restore your health.
Dr. Cook is concentrated on permanent or long-term treatments and approaches to my condition, instead of just throwing medications at my pain and wishing me luck.
-Christina

The lesser-known facts about endometriosis:
- Did you know that endometriosis can persist into menopause?
- Did you know that in very rare cases endometriosis has been found involving the lung, brain, eye, kidney and liver?
- Did you know that the oldest patient ever to be treated for endometriosis was in her 80s?
- Did you know that anecdotal reports of endometriosis date back to 1825 BC in the Kahun Papyrus in ancient Egypt?
- Did you know that endometriosis has been reported in stillborn female fetuses, prepubescent girls, men undergoing treatment for prostate cancer, and women born without a uterus?
UP NEXT: What happens when you have endometriosis?
Read Dr. Cook’s most shared article here: What it Really Means to Have Endometriosis.
Additional Endo Resources:
Follow us on Instagram
Join our Facebook conversation
Read Dr. Cook’s Books
What Causes Endometriosis?
At this point in time, we do not know what causes endometriosis. When considering the origin and manifestation of a disease we need to consider the factors that determine whether a woman develops the condition or not and, of those women who do develop the disease, the factors that determine how severe her disease ultimately is (how symptomatic, how aggressive, how invasive and how extensive). Until now several theories of the origin and disease manifestation of endometriosis have been proposed. The aim of a theory of origin is to present an explanation that adequately accommodates all that we know about the disease. Generally, the best-fit theory is adopted and used to guide and predict treatments and outcomes. Over time if new information becomes available the best-fit theory may be surpassed or replaced by another competing theory or alternatively may be adapted in order to accommodate the new findings.

Perhaps one of the most popular and enduring theories of origin is that of retrograde menstruation, transportation and implantation. This is the belief that endometriosis occurs through a process of endometrial tissue flowing back through the fallopian tubes during menstruation, entering the pelvic cavity and implanting and invading the surfaces of the pelvic structures.
Retrograde menstruation, however, is a common phenomenon that occurs in 90% of women yet only 10% of women develop endometriosis and the refluxed material only contains minimal deposits of endometrial tissue. Furthermore, endometriosis consists of tissue that is similar but not identical to the native endometrium that lines the uterus, suggesting that it is not a mere autotransplant. Other phenomena about the disease that cannot be adequately explained by this theory include the presence of endometriosis in stillborn female fetuses, in women without a functional uterus and in a small number of men undergoing treatment for prostate cancer. The theory of retrograde menstruation predicts that the disease will recur after surgery and worsen over time with each menstrual flow, yet surgical excision of endometriosis has been found to effectively remove the disease in most patients with true disease recurrence being rare. Studies examining the extent of disease across different age groups of patients have failed to find an increase in disease with age.
Research reveals that women with endometriosis are at increased risk of also having various autoimmune disorders, including allergies, systemic lupus erythematosus, Sjögren’s Syndrome, rheumatoid arthritis, and multiple sclerosis. Based on this finding a hybrid theory was developed that extends upon Sampson’s theory of retrograde menstruation. As mentioned above, retrograde menstruation occurs in around 90% of women yet only a minority ever develop endometriosis. It has been hypothesized that an underlying immune dysfunction interferes with the body’s natural ability to clear up this refluxed tissue from the pelvis and therefore the tissue is allowed to establish itself and proliferate, resulting in endometriosis. This line of argument suffers many of the same limitations as the original theory of retrograde menstruation. While autoimmune disorders are more common in women with endometriosis, many women with endometriosis do not have any such disorders. Another important question is whether immune dysfunction truly precedes the onset of endometriosis or rather is it a result of the disease process itself. Endometriosis triggers an ongoing immune response, which over time could moderate or disrupt immune function, altering an individual’s propensity to developing autoimmune disorders.
The theory of Mülleriosis is the notion that endometriosis is already laid down during embryonic development and remains dormant until later in life when changes in hormones (such as during puberty or pregnancy) trigger the disease to become active and symptomatic. During embryonic development tissue is laid down and differentiated into the various pelvic organs and structures that form the pelvis, including the reproductive organs. In women with endometriosis, something goes awry during this process and tissue that would ordinarily be restricted to the inside of the uterus ends up developing in locations outside the uterus. A helpful analogy is that of a chef who is following a recipe for a full course dinner. He has all of the right ingredients but the recipe contains mistakes and some of the ingredients that should belong in the starter end up in the desert and some ingredients intended for the dessert end up in the main course. In the development of the reproductive organs HOX genes determine which tissue develops where. It is possible that abnormalities in these genes, whether spontaneous or inherited, result in coding errors that in turn result in the presence of aberrant endometriotic tissue outside the uterus (endometriosis). This theory can explain why the disease has been observed in infants and prepubescent girls, as well as the presence of other types of aberrant tissue that may co-occur with endometriosis, such as endocervicosis (tissue similar to the cervix found outside the uterus) and endosalpingiosis (tissue similar to the lining of the fallopian tubes present outside the tubes). It could also help explain the unique patterning of the disease i.e. why it occurs more commonly in some locations than others. Interestingly, there is a pattern of abnormalities and anomalies, such as urinary tract and uterine anomalies, adenomyosis, fibroids, and peritoneal pockets that are significantly more common in patients with endometriosis. This syndrome of conditions could be explained by a common underlying pattern of “coding errors” that manifest during embryonic development.
The embryonic rest theory proposes that cells of Müllerian origin can persist within the peritoneal cavity and under certain circumstances induce the formation of endometriotic tissue. An embryonic rest is a remnant of embryonic tissue that has persisted beyond the embryonic phase of development. Cells of Müllerian origin are the embryonic cells that originally comprised the Müllerian duct, a structure that subsequently differentiated into the female reproductive organs (specifically the fallopian tubes, the uterus and part of the vagina). It is unknown, however, whether these cells really can persist beyond early life.
A recent theory is that endometriosis arises from endometrial stem cells located outside the uterus. Stem cells are undifferentiated cells that harbor the potential to regenerate and produce more differentiated “daughter” cells. It is proposed that stem cells located in the pelvis outside the uterus bring about the regeneration and differentiation of endometriotic lesions. These same cells play a role in the monthly regeneration of endometrial tissue inside the uterus after each menstrual flow.
In very rare cases a patient will present with endometriosis in far away places, such as the lung, the brain or even the eye. One explanation for these occurrences is that small amounts of endometrial tissue can spread throughout the body via the lymphatic and vascular system. It is unclear, however, how this process would occur and perhaps a more plausible explanation is that the disease presents in these distant sites due to a process of coelomic metaplasia (the transformation of cells or tissue from one type to another).
Coelomic metaplasia rests on the notion that any cell in the body has the potential to become any other cell. All cells have the same basic genetic code but are differentiated by the different ways in which their basic genetic code is expressed. The expression of any given cell’s genetic code may be influenced by any manner of factors (such as inflammation, exposure to toxins, and wound healing). In the case of endometriosis, the theory of coelomic metaplasia predicts that the genetic material in a cell or a group of cells (tissue) becomes expressed differently causing the tissue to transform into endometriosis. This theory could explain the occurrence of disease in distant sites in the body, scar endometriosis, and the presence of disease in men undergoing treatment for prostate cancer.
It has been found that endometriosis runs in families. A woman’s risk of developing the disease is significantly increased if her mother or sister also also has the disease. These findings point to a genetic origin of the disease. What we do know is that no individual gene is responsible for endometriosis and the pattern of inheritance is complex. Most likely a complex array of genes are involved in the familial transmission and expression of this disease and these genes may interact with environmental factors to determine disease extent and severity.
With an increase in exposure to toxins in the surrounding environment (air pollutants, toxic chemicals in household products and in the food chain) as well as increasing exposure to estrogens in the foods we consume it has been hypothesized that more women may develop endometriosis than previously or that the severity of endometriosis may be exacerbated by exposure to certain chemicals. There are two potential mechanisms through which environmental factors may play a role. Firstly there is the potential for dioxin exposure in vitro to result in genetic mutation, which in turn could cause the disease to occur, and secondly exposure to certain chemicals over the lifespan could enhance disease activity or even result in an underlying “latent” susceptibility to the disease becoming expressed. If an area of tissue harbors the potential to become endometriosis through metaplasia, an environmental factor could be the catalyst that triggers this change to occur. This brings up the role of epigenetics, which is when external factors alter the expression of a person’s genes. Alterations in gene expression can in turn result in changes in the behavior of cells in the body. It is important to note, however, that endometriosis has existed for millennia.
As you can see, various theories have been proposed to explain the origin and presentation of endometriosis. The question of what causes this disease and why some women present with more advanced and aggressive disease than others is far from simple. At this point in time we do not have all the answers. Most likely a complex interplay between several of the above described theories ultimately holds the key to fully unraveling the cause and in turn the cure of this enigmatic disease.
