Many women with endometriosis who suffer from pelvic pain will also have co-existing urogynecological disorders that contribute to their symptoms. Sometimes one disorder may mask other co-occurring disorders and it takes a skilled physician to correctly differentiate the many possible sources of pelvic pain.
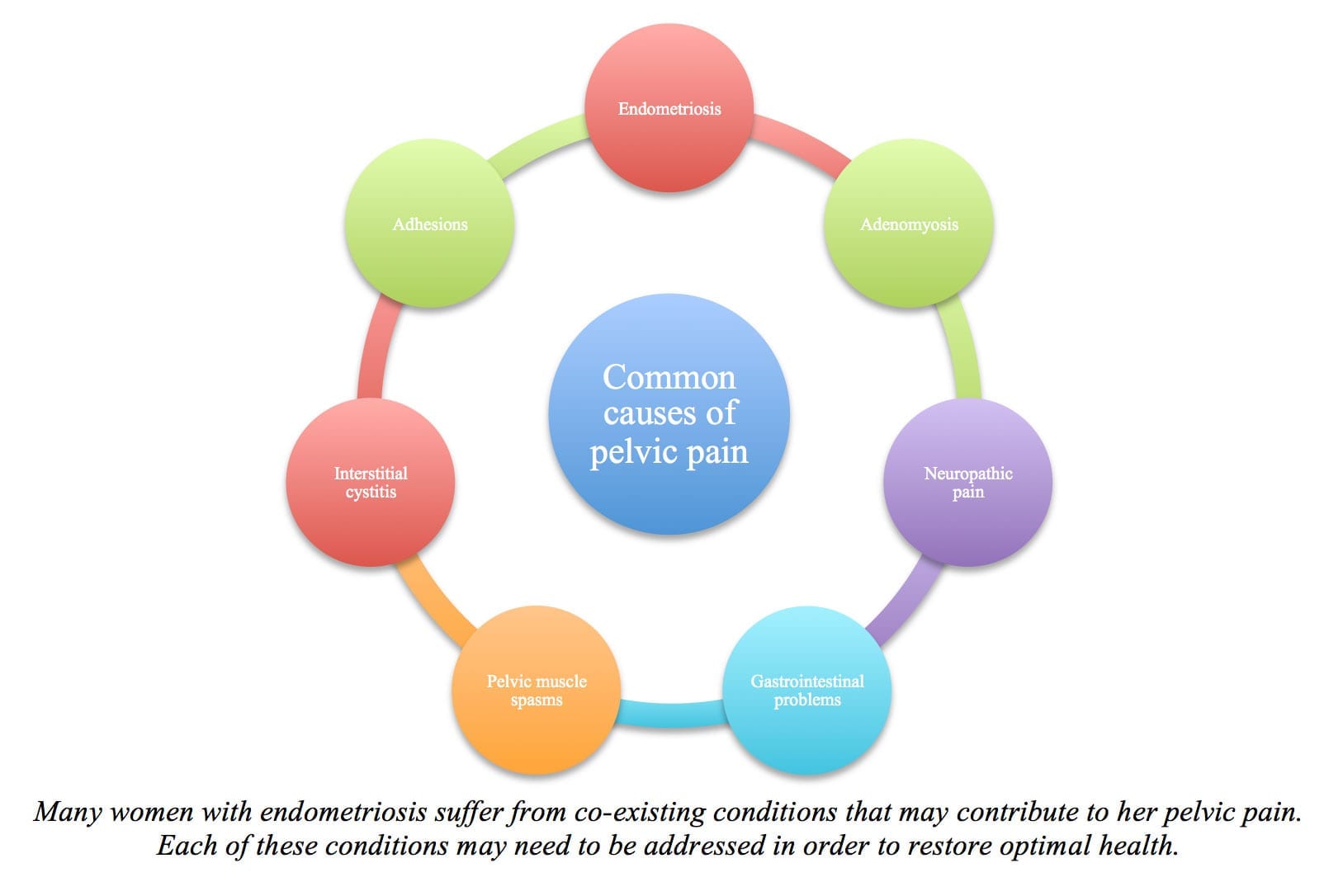
While endometriosis is a leading cause of pelvic pain, pelvic pain is often multifactorial in origin – it can stem from multiple causes.
The following conditions commonly co-occur with endometriosis and represent additional causes of pelvic pain: