The content contained in this web site is for informational use only and is not intended as medical advice. You should always seek the advice and care of your local physician. Information on this web site is also subject to change without notice and may include technical inaccuracies or typographical errors.
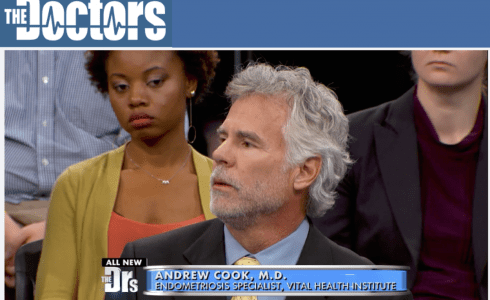
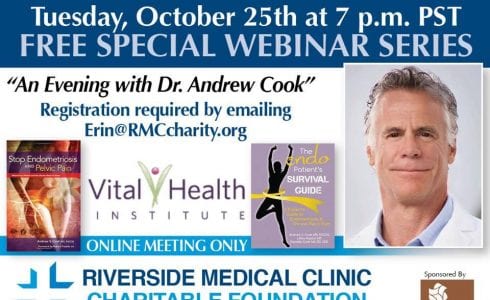
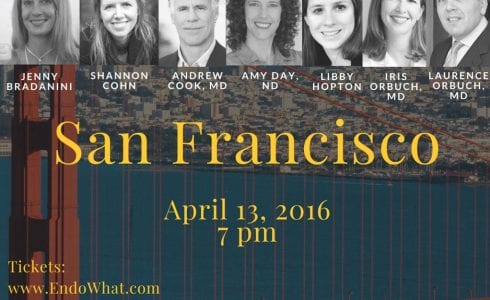
Vital Health Endometriosis Center is an international treatment center located in Durango, Colorado and specializes in endometriosis and chronic pelvic pain. Women travel from throughout the U.S., Canada and countries worldwide to Durango for treatment by Dr. Andrew Cook and his dedicated, professional staff.